
Microdosing cannabis may fight liver cancer and lower the risk of developing the disease. ElTelbany, et. al. (2022) found that patients with a history of cannabis use are 55% less likely to develop liver carcinoma than non-cannabis users.
Small amounts of cannabis exert potent anticancer properties: they inhibit the spread of cancer cells to other parts (metastasis) and induce cancer cell death (apoptosis), among other things.
A British Journal of Cancer article also suggests that “cannabinoids could be potential combination partners for established chemotherapeutic agents or other therapeutic interventions in cancer treatment.”
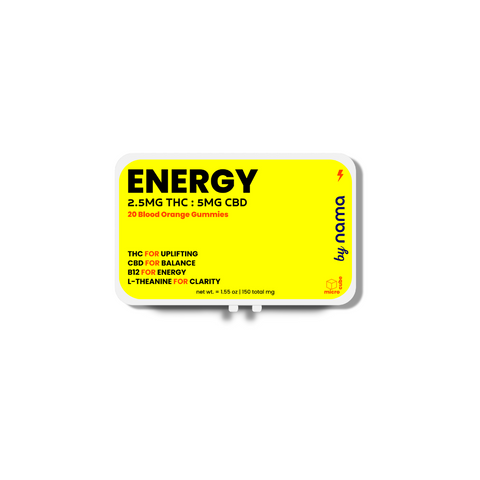
Our THC gummies provide a balanced low dose of THC and CBD to deliver the therapeutic benefits of cannabis without side effects. This makes them safe and effective for potentially fighting cancer and alleviating symptoms associated with cancer treatment.


THC: 10 mg | CBC: 10 mg | CBD: 10 mg | CBG: 5 mg | CBN 5mg
Understanding liver cancer
Liver cancer is a malignant growth that forms when normal liver cells develop mutations in their DNA. These mutations cause the cells to grow and divide uncontrollably, forming a tumor. Cancerous cells disrupt liver function and can spread to other parts of the body.
The liver is a vital organ with over 20 essential functions. Here are some of them:
- Detoxification: the liver filters toxins, drugs, and harmful substances from the blood
- Bile production: it produces bile to help digest fats in the small intestine
- Glucose regulation: the liver stores excess glucose as glycogen and releases it when needed
- Protein synthesis: it produces crucial proteins such as albumin and blood clotting factors
- Nutrient processing: it processes and stores essential nutrients
- Hormone metabolism: the liver breaks down and regulates thyroid hormones, cortisol, and sex hormones
- Immune support: the liver houses immune cells that fight infections and remove debris
- Cholesterol regulation: it synthesizes cholesterol, removes excess cholesterol, and converts it into bile acids
- Vitamin storage: it stores fat-soluble vitamins (A, D, E, and K) and copper
- Ammonia metabolism: it converts ammonia, a toxic byproduct of protein metabolism, into urea for excretion
Any disruption to these functions can lead to serious health consequences.
What are the symptoms of liver cancer?
Early-stage liver cancer often doesn't cause noticeable symptoms. As the disease progresses, more obvious and serious signs start to appear.
Here are some of the most common ways to recognize liver cancer:
- Abdominal pain and swelling
- Unexplained weight loss
- Jaundice
- Fatigue and weakness
- Nausea and vomiting
- White, chalky stools
- Fever
If you notice any of these symptoms, talk to your doctor right away.
Types of liver cancer
Liver cancer has several manifestations. The primary subtypes include the following:
- Hepatocellular carcinoma (HCC) is the most common type, accounting for about 75% of all cases. It develops in the main liver cells called hepatocytes. This liver type is often associated with chronic liver diseases, such as cirrhosis, hepatitis B, or hepatitis C.
- Intrahepatic cholangiocarcinoma (bile duct cancer) develops in the cells lining the bile ducts within the liver. It accounts for about 10–20% of all liver cancers. Risk factors for this type of liver cancer are primary sclerosing cholangitis (a chronic liver disease involving inflammation and scarring of the bile ducts), liver fluke infections (caused by parasitic flatworms that invade the liver and bile ducts), and certain congenital disorders.
- Angiosarcoma and hemangiosarcoma are rare types of liver cancer—they both account for about 1% of all liver cancer. They develop in the blood vessels of the liver. People exposed to certain chemicals, such as vinyl chloride and thorium dioxide, are more likely to develop these types. Prognosis is generally poor because these cancers are often diagnosed at an advanced stage
- Hepatoblastoma is a rare type that primarily affects children younger than 4 years old. It develops in immature liver cells called hepatoblasts. Certain genetic conditions are major risk factors for hepatoblastoma cancer. The prognosis is generally good if the disease is caught early.
- Secondary (metastatic) liver cancer occurs when cancer from another part of the body spreads to the liver. The most common types of cancer that spread to the liver are colorectal, breast, lung, and pancreatic cancers.
What are the risk factors for liver cancer?
Some environmental and lifestyle influences increase the chances of developing liver cancer. Risk factors include the following:
- Chronic viral hepatitis, such as hepatitis B virus (HBV) and hepatitis C virus (HCV) infections, are the leading causes of liver cancer worldwide. Chronic HBV or HCV infection can lead to cirrhosis and liver cancer.
- Cirrhosis is the scarring of the liver, which can happen because of alcohol abuse, fatty liver disease, and chronic viral hepatitis. Cirrhosis increases the risk of liver cancer, regardless of the underlying cause.
- Excessive alcohol consumption is a major risk factor for cirrhosis, which increases the risk of liver cancer. The risk is particularly high in people who have both alcohol abuse issues and chronic viral hepatitis.
- Non-alcoholic fatty liver disease (NAFLD) occurs when fat accumulates in the liver. This condition is often associated with obesity, diabetes, and metabolic syndrome. Advanced stages of NAFLD, such as non-alcoholic steatohepatitis (NASH) and NAFLD-related cirrhosis, increase the risk of liver cancer.
- Aflatoxin exposure may lead to liver cancer. Aflatoxins are toxic substances produced by certain types of mold that can grow on improperly stored food, such as grains and nuts.
- Inherited metabolic diseases, such as hemochromatosis (iron overload) and Wilson's disease (copper accumulation), may lead to cirrhosis and ultimately liver cancer.
- Type 2 diabetes, particularly when associated with obesity and NAFLD, has been linked to liver cancer.
- Obesity, which is a significant risk factor for NAFLD, NASH, and cirrhosis, makes a person more susceptible to liver cancer.
What treatments are effective against liver cancer?
Modern medicine has an arsenal of interventions to battle liver cancer. Treatments include the following:
- Surgery removes the tumor or part of the liver.
- Liver transplantation replaces the diseased liver with a healthy one from a donor.
- Ablation uses heat, cold, or chemicals to directly destroy cancer cells.
- Embolization involves blocking the blood supply to the tumor to starve it of nutrients.
- Targeted therapy uses drugs that specifically target cancer cell mechanisms to slow their growth and spread.
- Radiation therapy uses high-energy rays to kill cancer cells or shrink tumors.
Many of these treatments cause unpleasant side effects, which further degrade the quality of life for liver cancer patients. As a result, more and more people are seeking natural and safer alternatives to combat cancer and alleviate symptoms. One such alternative involves the consumption of low doses of cannabis.
Small amounts of cannabis (between 2 and 10 milligrams of THC per serving) have therapeutic benefits and fewer side effects than higher doses. This makes them safer and potentially more effective for treating many medical conditions such as migraines, chronic pain, anxiety, insomnia, and cancer.
How does cannabis fight cancer?
Emerging research reveals the potent anticancer effects of cannabinoids. The aforementioned systematic review and meta-analysis indicates the following anticancer mechanisms of Delta 9 THC and cannabidiol (CBD):
- THC and CBD stop cancer cells from multiplying by interfering with the signals that instruct the cells to divide. They block a key growth-promoting pathway called Akt and activate proteins such as p21 and p27 that act as "brakes" on the cell cycle.
- Cannabinoids trigger programmed cell death called apoptosis in cancer cells. These pathways include the buildup of the lipid molecule ceramide, stress in the endoplasmic reticulum (ER) where proteins are made, and the production of reactive oxygen species (ROS) that damage cancer cell components.
- THC and other cannabinoids cause cancer cells to undergo a form of self-digestion called autophagy, which often leads to cell death. They trigger cancer cell autophagy by suppressing the Akt/mTOR pathway, which normally promotes cell survival and growth, and activating AMPK, an enzyme that stimulates autophagy when cells are under stress.
- Cannabinoids upregulate TIMP-1, which inhibits specific proteins involved in cancer cell invasion. They also reduce the expression of Id-1, a key regulator of the invasive phenotype.
- Cannabinoids inhibit tumor angiogenesis by downregulating proangiogenic factors such as VEGF, PlGF, and Ang-2 produced by cancer cells. This starves tumors of the new blood vessels they require to grow.
- Cannabinoids stimulate anti-tumor immunity. They enhance the activity of lymphokine-activated killer cells against cancer cells.
- Cannabinoids may enhance the efficacy of conventional cancer treatments such as chemotherapy and radiation.
The review also emphasizes the role of the endocannabinoid system (ECS) in cancer progression. While our bodies naturally produce endocannabinoids, phytocannabinoids found in the cannabis plant interact with our ECS the same way endocannabinoids do. They bind to the CB1 and CB2 receptors to influence pain, sleep, appetite, the immune response, and many other biochemical changes in the body.
Cannabinoids also interact with cannabinoid receptors in the ECS to inhibit tumor angiogenesis, induce cancer cell apoptosis, and other antitumor properties.
Many cancer cells overexpress cannabinoid receptors, making them highly susceptible targets for cannabis compounds to activate cell death pathways. For example, Fraguas-Sánchez, et. al. discovered that human leukemia cells expressed high levels of CB2 receptors. Leukemic cells are rich in CB2 receptors that cannabinoids can target to induce cancer cell death.
This means that, through the endocannabinoid system, cannabis can fight leukemia and many other types of cancer.
How effective is cannabis against liver cancer?
Research shows that cannabis effectively fights liver cancer. Different cannabis compounds target specific receptors in the ECS to inhibit liver tumor growth, cause cancer cell apoptosis, and prevent the spread of malignant cells.
A 2019 study published in Biology Direct explained three important ways in which cannabis compounds fight hepatocellular carcinoma through the endocannabinoid system:
- Inhibiting HCC cell proliferation: MDA19, a compound that activates CB2 cannabinoid receptors, suppressed the growth of liver cancer cells in culture.
- Inducing apoptosis via the mitochondrial pathway: MDA19 treatment killed liver cancer cells by triggering apoptosis. It activated the mitochondrial apoptosis pathway, turning up proteins that promote cell death while turning down proteins that block it.
- Inactivating the AKT signaling pathway: MDA19 also blocked the AKT pathway in liver cancer cells, which normally promotes cell survival and growth. CB2 receptor inhibition reactivated the AKT pathway, showing that MDA19 turns off AKT signaling by turning on CB2.
Another study confirms what we already knew about the antitumor effects of cannabis. THC and a cannabis compound called JWH-015 activate the CB2 cannabinoid receptor to:
- Inhibit cancer cell proliferation
- Induce apoptosis
- Trigger autophagy
- Inhibit pro-growth AKT signaling
Iranian researchers found that CB1 agonists also show promising antitumor effects in fighting liver cancer. ACEA is a CB1 receptor agonist that works synergistically with cannabinoid CB65 (a CB2 receptor agonist) to downregulate the expression of MMP-2 and MMP-9, enzymes involved in breaking down the extracellular matrix that facilitates cancer cell invasion and metastasis.
Low doses of THC and CBD also work synergistically with cytotoxic chemicals to enhance their effectiveness against liver cancer. A 2023 study found that the combination treatment of cabozantinib and CBD enhances apoptosis in hepatocellular HCC cells. Together, they induce endoplasmic reticulum stress and activate the p53 pathway to trigger apoptosis in liver cancer cells and suppress tumor growth and progression.
These studies show that different cannabis compounds work together to fight liver cancer even more effectively than they would in isolation. When combined, THC, CBD, and other minor compounds enhance each other's therapeutic effects. Scientists refer to this synergistic action as the "entourage effect."
In the entourage effect, cannabis compounds work together in harmony. While THC and CBD are the most well-known, the hundreds of other cannabinoids, terpenes, and flavonoids in the plant also contribute to its synergistic action to fight liver and other types of cancer.
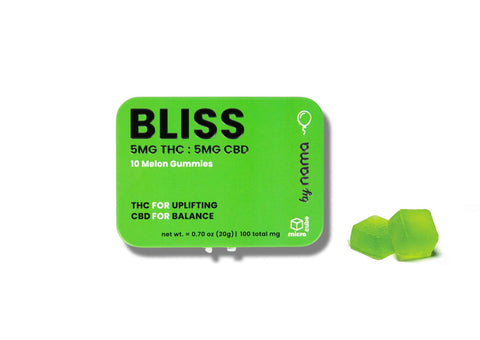
With a balanced blend of THC and CBD (10 mg per edible), our Euphoria gummies harness the entourage effect to combat liver cancer. Enjoy a burst of delightful flavors while experiencing the combined therapeutic relief.
“Didn’t review Euphoria in the sample review cause it’s my favorite!
It has a slow but steady good feeling.
And the taste is great. 👍🏼”
All of our full-spectrum CBD gummies gently elevate your mood without intoxication. Discover how our entourage effect edibles can be a powerful ally in the fight against liver cancer.
Product QUIZ
Need help deciding what product is best for you? Take our quiz, just three questions until your perfect match!
Cannabis for chemotherapy-related side effects
Chemotherapy and other treatments for liver cancer can be effective, but their adverse effects often worsen a patient’s quality of life. Many people find relief in a complementary therapeutic strategy—microdosing cannabis.
Canadian researchers explored how cannabis alleviates chemotherapy-related side effects mainly by upregulating the endocannabinoid system. Here’s what they found:
- THC and CBD are effective against nausea and vomiting caused by chemotherapy.
- They work together to stimulate appetite and prevent weight loss in patients with cancer undergoing treatment.
- Cannabinoids have analgesic properties. They relieve cancer-related pain and neuropathic pain caused by chemotherapy or radiation therapy.
- THC and CBD have anti-inflammatory properties. They may reduce inflammation associated with cancer and its treatment. This improves the overall condition and quality of life for cancer patients undergoing chemotherapy.
- Cannabis improves sleep quality, which is often disrupted in cancer patients because of chronic pain, anxiety, and other treatment-related side effects.
- Cannabis looks after your mental health, as well. Anxiety and depression are common in cancer patients undergoing treatment, but small amounts of THC and CBD lift off anxious thoughts and fight depression.
Our low-dose edibles are a natural way to combat these side effects, providing much-needed relief and improving the quality of life for liver cancer patients.
Why are low-dose edibles the best way to microdose cannabis?
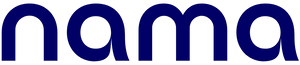
There are many different methods to consume cannabis, but not all of them are safe and effective, especially for medical purposes. That’s why many people choose our THC gummies and cannabis-infused beverages. Here’s why:
- The THC amount in our edibles and beverages is clearly labeled. This gives you control to accurately dose your drinks with our Buzz Drops™ and munch on our delicious gummies every time. You achieve the desired mild effects without overconsumption.
- When ingested, edibles are metabolized differently. The effects of gummies last between 6 and 8 hours, providing longer-lasting relief than inhalation methods.
- The effects of edibles also come on slowly, usually within 30 minutes to 2 hours.
- Edibles bypass the lungs entirely, avoiding any potential irritation or carcinogens associated with smoking or vaping. Isn’t this a much safer option, especially for those with respiratory issues or sensitivities?
- Low-dose edibles offer utmost discretion, with no telltale scents or smoke. If you’re microdosing cannabis for cancer, you can do that wherever you are without drawing attention.
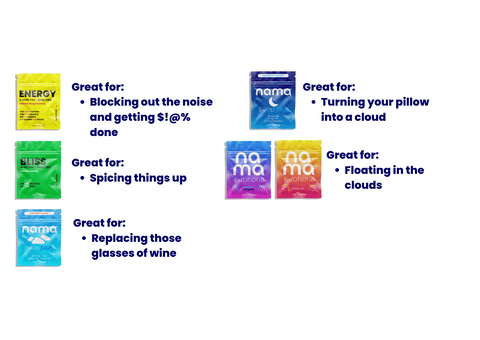
Ready to experience blissful microdosing? Try our Bliss Delta 9 gummies. They are the perfect low-dose option to help manage anxiety, improve sleep, and bring some fruity delight to your day.
The best THC gummies and drinks for microdosing
Many cannabis products on the market contain contaminants such as heavy metals, pesticides, fungi, and bacteria that can be harmful. These contaminants are not regulated or tested for safety and have been linked to toxic effects on the liver, kidneys, and nervous system.
If you’re already struggling with liver or other cancer types, you don’t need to bring more toxins into your body. Choose high-quality, lab-tested cannabis products and shop at nama™. Our products ensure safety and deliver measurable doses you can trust.
For a refreshing alternative to gummies, try one of our THC mocktail recipes you can make with our low-dose Buzz Drops™. These cannabis mixers are a discreet and delicious way to microdose cannabis. Add a dropper or two of our liquid drops to your favorite non-alcoholic beverage (or make one of our craft mocktails), and you’re good to go. Ride a smooth, mellow buzz that delivers much-needed relief to cancer patients and anyone looking to reap the therapeutic benefits of drinking cannabis.
Our gummies and THC beverages undergo rigorous quality control and independent lab testing to ensure they consistently meet the highest standards for purity and reliability.
See where you can buy our edibles in the U.S.
Cannabinoids from the cannabis plant have therapeutic benefits for liver health. Clinical studies indicate that CBD may have anti-inflammatory and antifibrotic effects, which could be beneficial for liver conditions such as fibrosis and hepatitis.
Korean researchers found that CBD reduces liver inflammation, oxidative stress, fat accumulation, fibrosis, and cell death, while Wang, et. al. explain that CBD can also reduce alcohol-induced liver fat accumulation, metabolic disruptions, and neutrophil-mediated damage.
Animal studies have demonstrated that cannabinoids can reduce liver damage and improve liver function in models of liver cancer.
CBD has been shown to inhibit certain liver enzymes, particularly cytochrome P450 enzymes, which are crucial for drug metabolism. This inhibition affects how the liver processes different medications, leading to altered drug levels in the body and an increased risk of adverse reactions.
A 2021 study showed that CBD has the potential to interfere with the metabolism and clearance of drugs that are substrates for P450 enzymes. When a drug and CBD are co-administered, CBD could increase the systemic exposure of the drug by reducing its metabolism by the inhibited P450 enzymes in the liver. In simpler terms, CBD can increase the level of drugs in the body by inhibiting (decreasing the activity of) the liver enzymes that normally break down and eliminate the drugs.
On average, CBD can remain in the liver for several days to a week after ingestion. Pilot studies have shown that CBD metabolites can be detected in the liver for up to a week post-administration, indicating a relatively long elimination half-life in hepatic tissue. The time CBD remains in the liver varies based on the dosage, frequency of use, metabolism, and individual liver function.
CBD is safer than alcohol for the liver and other health aspects. Chronic alcohol consumption is a well-known cause of liver damage, leading to conditions such as fatty liver, hepatitis, fibrosis, and cirrhosis. Alcohol is even a major risk factor for cancer. The National Cancer Institute explains that “most American adults aren’t aware of the link between alcohol consumption and cancer.”
CBD has potential hepatoprotective effects. It lacks the hepatotoxicity associated with alcohol, which makes it a much safer option. Previous studies have also highlighted that CBD can aid in pain control and supportive care for patients with liver conditions.
The liver processes cannabinoids, primarily through the cytochrome P450 enzyme system. This enzymatic pathway metabolizes THC and CBD into their respective metabolites, which are then excreted from the body. The liver's role in metabolizing cannabinoids influences their pharmacokinetics and efficacy, as well as the potential for drug interactions.
Cannabinoid receptors, specifically CB1 and CB2 receptors, are present in the liver. These receptors play roles in many important physiological processes, such as the regulation of inflammation, fibrosis, and metabolic functions. When cannabinoids activate these receptors, they can promote liver health and inhibit disease progression.
Smoking has a detrimental effect on liver health. It can exacerbate liver diseases, such as non-alcoholic fatty liver disease (NAFLD), and increase the risk of liver cancer. Smoking cannabis also carries potential risks due to the inhalation of combustion by-products, although its direct impact on the liver is less well-documented compared to tobacco.
If you stick to low-dose edibles such as our THC gummies, you’re avoiding the health risk of damaging your lungs and further deteriorating your liver health.
Top Sellers
New? Start with our Ultimate Sampler!

THC: 10 mg | CBC: 10 mg | CBD: 10 mg | CBG: 5 mg | CBN 5mg
Resources
ElTelbany A, Khoudari G, Al-Khadra Y, McCullough A, Alkhouri N. Lower Rates of Hepatocellular Carcinoma Observed Among Cannabis Users: A Population-Based Study. Cureus. 2022 Apr 28;14(4):e24576. doi: 10.7759/cureus.24576. PMID: 35651376; PMCID: PMC9138632.
Hinz, B., & Ramer, R. (2022). Cannabinoids as anticancer drugs: Current status of preclinical research. British Journal of Cancer, 127(1), 1-13. https://doi.org/10.1038/s41416-022-01727-4
Fraguas-Sánchez, A. I., Martín-Sabroso, C., & Torres-Suárez, A. I. (2018). Insights into the effects of the endocannabinoid system in cancer: A review. British Journal of Pharmacology, 175(13), 2566-2580. https://doi.org/10.1111/bph.14331
Rao, M., Chen, D., Zhan, P., & Jiang, J. (2019). MDA19, a novel CB2 agonist, inhibits hepatocellular carcinoma partly through inactivation of AKT signaling pathway. Biology Direct, 14(1). https://doi.org/10.1186/s13062-019-0241-1
Vara, D., Salazar, M., Guzmán, M., & Velasco, G. (2011). Anti-tumoral action of cannabinoids on hepatocellular carcinoma: Role of AMPK-dependent activation of autophagy. Cell Death & Differentiation, 18(7), 1099-1111. https://doi.org/10.1038/cdd.2011.32
Pourkhalili, N., Ghahremani, M. H., Farsandaj, N., Tavajohi, S., Majdzadeh, M., Parsa, M., Lavasani, N. J., & Ostad, S. N. (2012). Evaluation of anti-invasion effect of cannabinoids on human hepatocarcinoma cells. Toxicology Mechanisms and Methods, 23(2), 120–126. https://doi.org/10.3109/15376516.2012.730559
Jeon, Y., Kim, T., Kwon, H., Kim, K., Park, T., Ham, J., & Kim, J. (2023). Cannabidiol Enhances Cabozantinib-Induced Apoptotic Cell Death via Phosphorylation of p53 Regulated by ER Stress in Hepatocellular Carcinoma. Cancers, 15(15). https://doi.org/10.3390/cancers15153987
Cherkasova, V., Wang, B., Gerasymchuk, M., Fiselier, A., Kovalchuk, O., & Kovalchuk, I. (2022). Use of Cannabis and Cannabinoids for Treatment of Cancer. Cancers, 14(20). https://doi.org/10.3390/cancers14205142
Chen, S., & Kim, K. (2024). The Role of Cannabidiol in Liver Disease: A Systemic Review. International Journal of Molecular Sciences, 25(4). https://doi.org/10.3390/ijms25042370
Wang, Y., Mukhopadhyay, P., Cao, Z., Wang, H., Feng, D., Haskó, G., Mechoulam, R., Gao, B., & Pacher, P. (2017). Cannabidiol attenuates alcohol-induced liver steatosis, metabolic dysregulation, inflammation and neutrophil-mediated injury. Scientific Reports, 7(1), 1-12. https://doi.org/10.1038/s41598-017-10924-8
Akinloye, D. I., Metibemu, D. S., Shittu, M. T., Lawal, M. A., Olatunji, F. O., Oyediran, M. A., & Akinloye, O. A. (2023). Cannabis sativa demonstrates anti-hepatocellular carcinoma potentials in animal model: In silico and in vivo studies of the involvement of Akt. Journal of Cannabis Research, 5. https://doi.org/10.1186/s42238-023-00190-z
Nasrin, S., Watson, C. J., Perez-Paramo, Y. X., & Lazarus, P. (2021b). Cannabinoid Metabolites as Inhibitors of Major Hepatic CYP450 Enzymes, with Implications for Cannabis-Drug Interactions. Drug Metabolism and Disposition/DMD Online, 49(12), 1070–1080. https://doi.org/10.1124/dmd.121.000442
Abbotts KSS, Ewell TR, Butterklee HM, Bomar MC, Akagi N, Dooley GP, Bell C. Cannabidiol and Cannabidiol Metabolites: Pharmacokinetics, Interaction with Food, and Influence on Liver Function. Nutrients. 2022 May 21;14(10):2152. doi: 10.3390/nu14102152. PMID: 35631293; PMCID: PMC9144241.
nama CBD FDA & legal disclaimer
Our products are not intended to diagnose, treat, cure, or prevent any disease. They are not a replacement for prescription medications and have not been evaluated by the U.S. Food and Drug Administration (FDA).
The information provided on this website does not and is not intended to, constitute legal advice or any statement of the status of any laws. Any information, content, and materials available on this site are for general informational purposes only and are not intended to be relied upon for any purpose.
Readers of this website should contact their attorney to obtain advice concerning any particular legal matter, including decisions on what products are, or are not, legal to sell, possess, or consume. No reader, user, or browser of this site should act or refrain from acting based on the information on this site without first seeking legal advice from their counsel in the relevant jurisdiction.
Further reading
What are the benefits of hybrid-strain cannabis?
Microdosing cannabis for bladder cancer
How much THC should I microdose?
What are the ingredients of Buzz Drops™?
Microdosing Delta 9 for Parkinson’s disease
About
Learn
Join us on this journey
© Copyright 2026 nama Products LLC. All Rights Reserved.
†These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease. All information presented here is not meant as a substitute for or alternative to information from health care practitioners. Please consult your health care professional about potential interactions or other possible complications before using any product.
††The information provided on this website does not, and is not intended to, constitute legal advice or any statements of the status of any laws. Any information, content, and materials available on this site are for general entertainment purposes only, and are not intended to be relied upon for any purpose.

By clicking ‘Yes,’ you agree to our
Terms & Conditions and Privacy Policy
123 John Doe Street
Your Town, YT 12345
Store Hours
Sun: Closed
Mon-Fri: 9:00 - 17:00
Sat: 10:00 - 13:00
What to expect at pickup
Closed
Closing at 5pm
Closing at 5pm
Closing at 5pm
Closing at 5pm
Closing at 5pm
Closing at 1pm

![Buzz Packs™ [THC and CBD Powder Drink Mix]](http://www.namacbd.com/cdn/shop/files/nama_buzz_packs_thc_drink_pack_white_background.png?v=1769586244&width=480)
![Buzz Packs™ [THC and CBD Powder Drink Mix]](http://www.namacbd.com/cdn/shop/files/Buzz_Packs_Label.png?v=1769586244&width=480)












![Buzz Drops™ [THC Drink Drops]](http://www.namacbd.com/cdn/shop/files/nama_thc_buzz_drops.png?v=1711412866&width=480)
![Buzz Drops™ [THC Drink Drops]](http://www.namacbd.com/cdn/shop/files/buzz-drop-wine-comparison.png?v=1736882023&width=480)





Comments (0)
There are no comments for this article. Be the first one to leave a message!